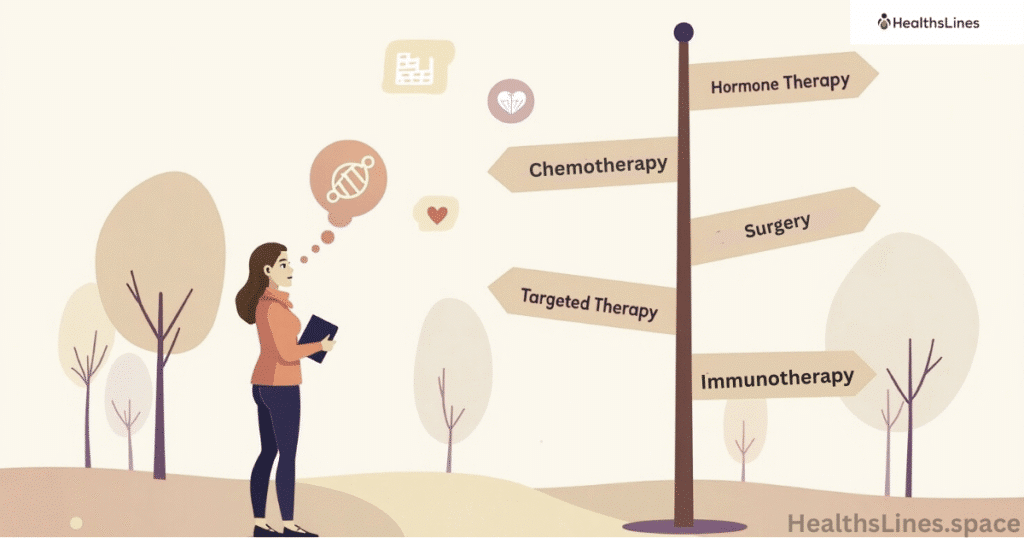
Choosing first-line breast cancer therapy is one of the most important decisions you’ll make after diagnosis. This first treatment can set the stage for your entire recovery plan. But not every patient needs the same approach. The best therapy depends on the type of cancer, stage, receptor status, overall health, and personal preferences.
Some breast cancers grow slowly. Others spread quickly and need aggressive treatment right away. Understanding your cancer helps you choose the best first-line treatment for breast cancer based on medical facts, not fear. The goal is to stop the cancer, keep you strong, and protect your quality of life.
Cancer Type Decides the First Treatment
Your doctor first checks if the breast cancer is noninvasive, invasive, or metastatic. Noninvasive breast cancer, like ductal carcinoma in situ (DCIS), stays in the ducts. It usually needs surgery and sometimes radiation therapy after surgery. Invasive cancers spread beyond the ducts and need more serious treatment.
If cancer has spread to other organs, it becomes metastatic breast cancer (MBC). At this stage, treatment isn’t about a cure but about control and comfort. This is when metastatic breast cancer first-line therapy becomes vital. Doctors often use targeted therapy, hormonal drugs, or chemotherapy for breast cancer, depending on the cancer’s features.
Hormone Receptor-Positive Breast Cancer Treatment
If your breast cancer is hormone receptor-positive (HR+), it means the cancer cells grow in response to the hormones estrogen (ER-positive) or progesterone (PR-positive). This type makes up about 70% of all breast cancer cases. The first-line treatment usually involves hormonal therapy, which blocks or lowers hormone levels in the body to slow or stop cancer growth.
For premenopausal women, doctors often prescribe tamoxifen, a selective estrogen receptor modulator. It prevents estrogen from attaching to cancer cells. In postmenopausal women, aromatase inhibitors like anastrozole, letrozole, or exemestane are more common First-Line Breast Cancer Therapy. These drugs stop the body from making estrogen altogether.
In advanced or metastatic HR+ breast cancer, hormonal therapy is often combined with CDK4/6 inhibitors like palbociclib (Ibrance), ribociclib (Kisqali), or abemaciclib (Verzenio). These drugs help prevent cancer cells from dividing and spreading. This combination has significantly improved survival rates and delayed the need for chemotherapy in many patients.
Doctors may also use ovarian suppression therapy, especially in younger women, to stop the ovaries from producing estrogen. In some high-risk cases or when hormone therapy fails, chemotherapy might be added.
The treatment plan depends on menopausal status, tumor size, spread, genetic markers, and overall health. HR+ breast cancer is often slow-growing and responds well to hormonal therapies, which means many patients can avoid more aggressive treatments early on.
Staying consistent with medication and follow-up is key to long-term success and recurrence prevention.
HER2-Positive Breast Cancer Therapy Options
Cancers with high levels of the HER2 protein grow fast. But today, we have great treatments. The standard treatment plan for HER2+ breast cancer includes trastuzumab and pertuzumab combined with chemo. This is known as the trastuzumab pertuzumab chemo combination.
Doctors often give this mix as neoadjuvant therapy, before surgery, to shrink tumors. Then, adjuvant therapy continues after surgery to kill any remaining cancer cells. These drugs target HER2 directly, slowing or stopping growth.
Triple-Negative Breast Cancer Treatment Options
Triple-negative breast cancer (TNBC) is an aggressive form of breast cancer that doesn’t have estrogen receptors, progesterone receptors, or HER2 proteins. Because it lacks these targets, TNBC doesn’t respond to hormone therapy or HER2-targeted treatments. Instead, it requires a different and often more aggressive approach.
The main treatment for TNBC is chemotherapy, which is typically given either before surgery (neoadjuvant) to shrink the tumor or after surgery (adjuvant) to kill any remaining cancer cells. Common chemotherapy drugs include anthracyclines and taxanes, which are often used in combination for better results.
In recent years, immunotherapy has shown promise for TNBC. The FDA has approved atezolizumab (Tecentriq) in combination with chemotherapy for certain patients whose cancer expresses the PD-L1 protein. Immunotherapy helps the immune system recognize and destroy cancer cells more effectively First-Line Breast Cancer Therapy.
PARP inhibitors like olaparib (Lynparza) are also used for TNBC patients who have BRCA1 or BRCA2 mutations. These drugs block a repair pathway in cancer cells, causing them to die.
Due to its fast-growing nature and higher risk of recurrence, TNBC often requires close monitoring and follow-up. Clinical trials are also a valuable option for access to emerging treatments and should be considered early in the treatment plan.
First-Line Therapies for Metastatic Breast Cancer
Metastatic breast cancer (MBC) means the cancer has spread beyond the breast to other parts of the body like bones, liver, lungs, or brain. While it’s not considered curable, many patients live for years with the right treatment. The goal of first-line therapy is to control the disease, ease symptoms, and maintain quality of life.
For hormone receptor-positive (HR+) MBC, the first-line treatment is often hormonal therapy combined with a CDK4/6 inhibitor like palbociclib, ribociclib, or abemaciclib. This helps slow down the cancer’s growth while minimizing side effects.
For HER2-positive MBC, targeted therapy with trastuzumab and pertuzumab, often paired with chemotherapy, is the standard approach. It targets the HER2 protein and helps extend survival.
Triple-negative MBC is harder to treat. Chemotherapy is usually the first step, but if the tumor expresses PD-L1, immunotherapy like atezolizumab or pembrolizumab may be added.
Doctors base their recommendations on the cancer’s features, past treatments, and the patient’s health and preferences.
When to Use Chemotherapy for Breast Cancer First
Chemotherapy for breast cancer is strong medicine. It kills fast-growing cells, including cancer. But it also affects healthy cells, causing side effects like fatigue, nausea, and hair loss. So, doctors only use it when it offers real benefits.
Chemo is often the first step for triple-negative, HER2-positive, or high-grade tumors. It’s also used when cancers are large, fast-growing, or in lymph nodes. It may be given before surgery (neoadjuvant) or after (adjuvant), depending on your treatment plan.
Is Surgery or Radiation First for Early-Stage Cancer?
For early-stage breast cancer, surgery is usually the first step in treatment. The goal is to remove the tumor entirely, often through lumpectomy (breast-conserving surgery) or mastectomy (removal of the whole breast). The choice depends on the tumor’s size, location, and the patient’s overall health and preferences.
Radiation therapy typically follows surgery, especially after a lumpectomy, to kill any leftover cancer cells and reduce the risk of recurrence. However, in certain cases, such as when a tumor is too large or in a difficult location, doctors might recommend radiation before surgery to shrink the tumor and make it easier to remove.
The sequence depends on many factors—tumor characteristics, genetics, and patient preferences. A multidisciplinary cancer care team works together to decide the best course of action. Personalized treatment plans are essential to achieving the best possible outcome in early-stage breast cancer.
Targeted Therapy for Breast Cancer Based on Genetics

Sometimes, cancer has special gene changes. These can be found using genomic testing like Oncotype DX or the FoundationOne test. These tests help doctors decide if you need chemo or if other drugs will work better.
If you have a BRCA mutation, your doctor might use PARP inhibitors. These drugs target broken DNA repair systems in cancer cells. Other targeted therapy for breast cancer includes drugs for PIK3CA mutations or androgen receptors. The goal is a personalized breast cancer treatment plan based on your cancer’s exact traits.
What Affects the Right Treatment Plan for You
Doctors don’t use a one-size-fits-all approach. Several things guide the decision:
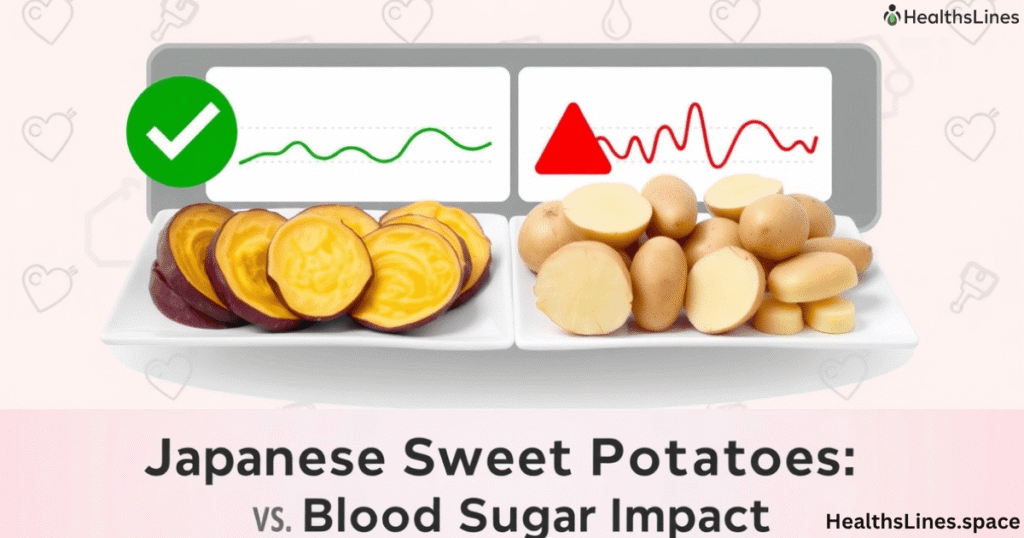
| Factor | How It Affects Treatment |
| Age & Menopausal Status | Affects hormonal therapy choices |
| Tumor Size & Grade | Determines if chemo or surgery is first |
| Lymph Node Involvement | May require chemo or radiation |
| Receptor Status (ER, PR, HER2) | Direct therapy type (hormonal, HER2, etc.) |
| Genetic Mutations (BRCA) | Opens options for PARP inhibitors |
| Overall Health & Other Illnesses | Affects drug choice and treatment intensity |
These help doctors choose the best first-line treatment for breast cancer that fits your unique case.
Questions to Ask Your Oncologist About Treatment
Before you start, talk openly with your care team. Good questions help you understand your path. Some smart ones to ask:
What type of breast cancer do I have? What’s the goal of this treatment? Will I need chemo, surgery, or radiation first? What are the side effects? How can we manage them? Are there clinical trials for breast cancer I can join? What’s my long-term outlook with this plan?
Asking the right questions to ask your oncologist breast cancer gives you control and confidence.
Real Case Examples That Show Treatment Differences
Case 1: Maria, 43, has ER-positive breast cancer. She gets surgery first, then takes letrozole with palbociclib. No chemo needed, and her Oncotype DX score was low.
Case 2: Jamie, 52, has HER2-positive breast cancer with a 3 cm tumor. Doctors give trastuzumab, pertuzumab, and chemo before surgery. The tumor shrinks, and she has a lumpectomy followed by more HER2 therapy.
Case 3: Sasha, 38, has triple-negative breast cancer with a BRCA mutation. She starts with chemo and pembrolizumab. After surgery, she begins PARP inhibitor therapy to reduce risk of return.
These real cases show why treatment must fit each person, not just the diagnosis.
Stay Involved and Informed About Your Treatment
It’s your body and your future. You deserve to know what’s going on and why. Ask questions. Get second opinions. Read from trusted sources like the NCCN breast cancer guidelines or ASCO treatment recommendations.
Join support groups. Talk to survivors. Explore clinical trials for breast cancer. Today’s science offers more tools than ever before to tailor your care. Staying active in your plan helps improve your outcome and peace of mind.
Conclusions
The first-line breast cancer therapy you choose will shape your journey. It must match your type of cancer, your health, and your goals. Whether it’s hormonal therapy, chemo, HER2-targeted drugs, or immunotherapy, the goal is the same: to stop the cancer while protecting your life.
Ask questions. Get the facts. And work with your team to find the personalized breast cancer treatment plan that fits you best. Because in cancer care, one size never fits all.